The history of 5DCT
The unreliability and qualitative nature of 4DCT was the driving force for Dr. Low to develop a replacement technique. In the early 2000s, Dr. Low understood that the assumptions that breathing motion could be described as a function of time or phase and that the image data could be reliably acquired in a few seconds were the 4DCT process were fundamentally flawed. Developing a replacement was not a quick process. Early work focused on the use of cine scanning, the process of acquiring repeated CT scans at a single location and then moving the scanner to the abutting region, which still suffered from the problem that images were taken for a relatively short period of time.
The fist breakthrough was the concept that an equation could be used to reliably describe human breathing motion. Other investigators had described the use of a model for breathing motion characterization, but they retained the concept that the motion model was based on time, and it was clear that time was not a useful variable given breathing irregularity. Dr. Low considered that the patient-specific model variables had to not depend on time and that the time-dependency had to be explicit in a non-invasive breathing surrogate. Given that breathing itself could be described by a pneumotachometer measuring tidal volume (by integrating airflow). Tidal volume made sense as a time-dependent surrogate because the lung tissues would expand and move as a function of tidal volume.
While tidal volume could be used to describe motion, it was by itself insufficient to describe motion in general. It had been determined and reported by a team at Hokkaido University that the motion of tumors could differ between inhalation to exhalation1,2. This would not be possible with just the tidal volume, since the same tidal volume would occur during inhalation and exhalation and yet the tumor would be in two different places. Dr. Low hypothesized that the reason for hysteresis was pressure imbalances in the lungs during the act of respiration. Because the goal was to develop a non-invasive surrogate, using the pressure distribution as one of the surrogates was not possible, so Dr. Low further hypothesized that for quiet respiration, the pressure imbalance was always proportional, that is to say the relative imbalances were constant, and they were proportional to the excess pressure or vacuum in the trachea. Since measuring the air pressure in the trachea would be somewhat invasive, Dr. Low made a further approximation that the trachea pressure was proportional to airflow. Therefore, the surrogate responsible for breathing motion was the breathing amplitude as measured by tidal volume and the surrogate responsible for hysteresis was the breathing rate as measured by airflow. A quantity and its time derivative are called a phase space. The techniques that followed were termed 5DCT based on three spatial variables along with breathing amplitude and breathing rate.
Now that the two time-dependent surrogates had been selected, the next question was what form would the motion model take? In order not to over-fit the model, it was decided to make the model as mathematically simple as possible and modify the model as needed.
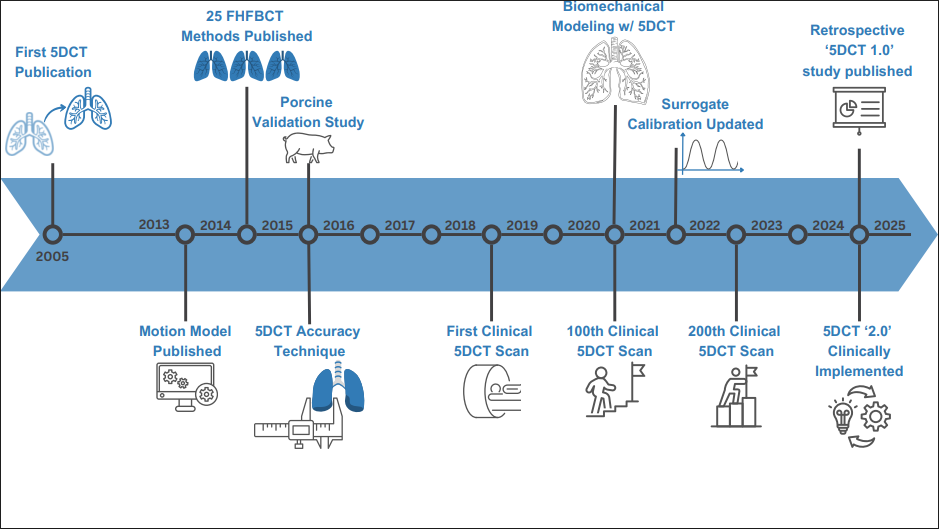
This model was originally published in 2005, 20 years ago3. The model described the motion of each location in the patient as a function of the breathing amplitude and rate. The mathematical form of the function was the simplest possible, the impact of the breathing depth and speed on the motion were linear and separated. The published form used the variables v and f to describe the tidal volume and airflow, but we have switched to the more general amplitude A and rate A ̇. The position of each voxel in the patient (including and especially in the lungs) X ⃗ was
X ⃗= (X_0 ) ⃗+α ⃗((X_0 ) ⃗ )A(t)+β ⃗((X_0 ) ⃗ ) A ̇(t)
The location has three terms, a constant and two that are functions of time. The amplitude and rate are functions of time and express the surrogate values that are measured or simulated depending on what the motion model is being used for.
The motion model was first used on cine scans, where 25 low-dose scans would be acquired at each couch position, then moving to the abutting couch position to repeat the process. This protocol was not practical for clinical use and matching the motion between abutting couch positions was challenging.
A breakthrough came in 2013, when it was realized that normal helical CT protocols could be used instead4,5. The cine scans were acquired rapidly and continuously, so they provided motion information in a series of snapshots for a few seconds. However, helical scans each require a few seconds to acquire, and the patient continued to breath during the scans. This meant that the lung apex might be scanned at peak inhalation while the diaphragm scanned at peak exhalation. In normal circumstances, interpreting these scans would be difficult since they did not reflect any specific breathing phase. However, their purpose was not to provide the lung images at particular phases, but to record the tissue positions as they scans progressed. The breathing amplitude and rate were synchronized to the scan acquisition, so the tissue locations could be correlated with the breathing surrogates and the surrogates themselves were assigned to each CT slice.
This breakthrough allowed the 5DCT workflow to become practical. CT acquisition became a series of 25 back-to-back CT scans, with a minimum vendor-mandated pause of 2s between scans. Because the scanners were relatively fast and breathing motion relatively slow, the images themselves had few blurring or other artifacts, although for particularly fast breathing patients and in parts of the lungs that moved quickly, motion-induced artifacts could indeed be visualized.
The model is built by conducting image registration of 25 free-breathing CT scans and one of those is selected as the reference scan. The reference scan may be the first scan or may be selected using other criteria, but for purposes of this description, it is the scan against which the others are compared using deformable image registration (DIR). Therefore, zero deviation is zero with respect to the reference scan. Equation 1 has three patient-specific parameters: (X_0 ) ⃗, α ⃗((X_0 ) ⃗ ) and β ⃗((X_0 ) ⃗ ). These need to be determined for each location (voxel) in the reference image. They are derived from the deformations measured when DIR is conducted on the CT scans. For each voxel, there are 25 values of the deformation in X, Y, and Z each. For each of these three directions, those deformations, along with their synchronized breathing amplitudes and rates, are used to determine the values of (X_0 ) ⃗, α ⃗((X_0 ) ⃗ ) and β ⃗((X_0 ) ⃗ ). Each component of these vectors is determined independently from the respective DIR components.
Since the reference scan is being acquired while the patient is breathing, the locations of the patient’s tissues within that scan do not reflect any specific breathing phase, so if the model was made relative to that scan, it would have little value. Instead, the model is made relative to a specific breathing amplitude and rate, 0 for each. Examining equation 1 and setting A and A ̇ = 0, we see that the tissue voxels appear at the locations (X_0 ) ⃗, imparting the meaning that the values of (X_0 ) ⃗ are used to transform the reference image to an image that reflects A and A ̇ = 0, which we term the reference breathing phase. While A ̇ = 0 is intuitive (breathing rate of 0, the equivalent of no airflow), the same is not true for A = 0. What is meant by a breathing amplitude of zero? There is no consensus or standard for this, so we have decided to define A = 0 as the 5th percentile breathing amplitude.
The model fit residual, specifically the root-mean squared displacement between the motion model and the DIR-based tissue positions was used as a metric for 5DCT precision. Because specific DIR errors could be correlated with breathing amplitude, the RMS residuals were not considered a measurement of accuracy, so there remained the chance that the 5DCT model, and consequently the CT images sent to treatment planning, could have significant errors. This was rectified in 2013 by Dou et al.6 when they realized that the original FHFBCT scans were ground truth measurements of tissue displacement and that the 5D motion model could be used to predict those scans. This provided a method for measuring the overall accuracy of the 5DCT approach, eventually leading to the clinical introduction of the technique in 2020. Prior to the clinical introduction, O’Connell et al conducted an AAPM TG100 safety analysis of the software and workflow.7
There have been some publications showing the overall precision and accuracy of the 5DCT process, and a recent manuscript by Lauria et al8 describing the early clinical experience with the 5D approach. More recently, we developed some updates to the 5DCT approach, and these will be published soon.
References
- Seppenwoolde Y, Shirato H, Kitamura K, et al. Precise and real-time measurement of 3D tumor motion in lung due to breathing and heartbeat, measured during radiotherapy. Int J Radiat Oncol Biol Phys. 2002;53(4):822-834.
- Shirato H, Seppenwoolde Y, Kitamura K, Onimura R, Shimizu S. Intrafractional tumor motion: lung and liver. Semin Radiat Oncol. 2004;14(1):10-18.
- Low DA, Parikh PJ, Lu W, et al. Novel breathing motion model for radiotherapy. Int J Radiat Oncol Biol Phys. 2005;63(3):921-929.
- Low DA, White BM, Lee PP, et al. A novel CT acquisition and analysis technique for breathing motion modeling [published online ahead of print 20130502]. Phys Med Biol. 2013;58(11):L31-36. PMC3685480
- Thomas D, Lamb J, White B, et al. A novel fast helical 4D-CT acquisition technique to generate low-noise sorting artifact-free images at user-selected breathing phases [published online ahead of print 20140307]. Int J Radiat Oncol Biol Phys. 2014;89(1):191-198. PMC4097042
- Dou TH, Thomas DH, O’Connell DP, Lamb JM, Lee P, Low DA. A Method for Assessing Ground-Truth Accuracy of the 5DCT Technique [published online ahead of print 20150807]. Int J Radiat Oncol Biol Phys. 2015;93(4):925-933. PMC4634638
- O’Connell D, Thomas DH, Lewis JH, et al. Safety-oriented design of in-house software for new techniques: A case study using a model-based 4DCT protocol [published online ahead of print 20190218]. Med Phys. 2019;46(4):1523-1532.
- Lauria M, Kim M, O’Connell D, et al. A Retrospective Analysis of the First Clinical 5DCT Workflow. Cancers. 2025;17(3).
Daniel Low, PhD
UCLA, Medical Physicist